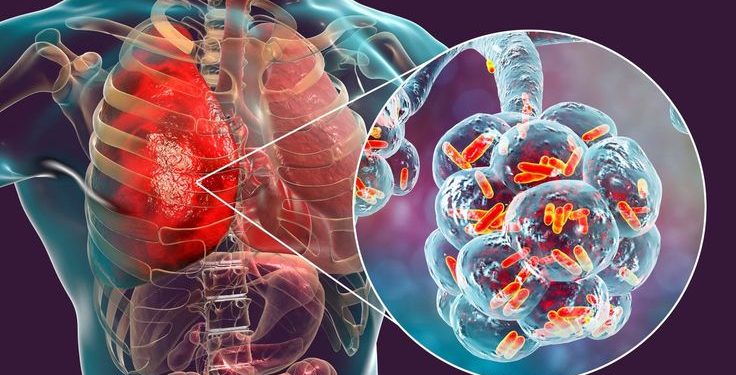
Jakarta, Indonesia Sentinel — Indonesia is still grappling with a serious tuberculosis (TB) cases crisis. According to the latest government figures, reporting an estimated 1.09 million cases and 125,000 related deaths.
Indonesia now ranks second in the world for tuberculosis cases, trailing only India, which recorded 2.8 million cases and 315,000 deaths.
The scale of the crisis not only underscores the threat of infectious diseases but also highlights deeper challenges within the healthcare system. Most notably, a shortage of specialist doctors, particularly pulmonologists and clinical microbiologists.
Deputy Health Minister Dante Saksono Harbuwono emphasized that one of the key obstacles in tackling TB, especially drug-resistant forms, is the lack of trained pulmonologists in many regions.
“Why do we need a pulmonary specialist in every district or city? Because when it comes to treating lung diseases especially drug-resistant TB we require skilled specialists to manage these complex cases,” said Dante during an interview in East Jakarta on Thursday (June 12), as reported by DetikHealth.
Ideally, every district or municipality in Indonesia should have at least one pulmonary specialist to ensure equitable access to referrals and proper treatment, particularly for patients with complicated TB cases.
Read Also:
Type 1 Diabetes Among Indonesian Children Continue to Rise, Reaches Nearly 2.000 Cases
The shortage extends beyond pulmonology. Arianti Anaya, Chair of the Indonesian Health Council (KKI), said the country is also facing a critical gap in clinical microbiologists, who are essential for diagnosing TBC through lab-based testing such as cultures, molecular rapid tests, and drug-resistance screening.
“To date, we have only 367 clinical microbiologists. We actually need 1,252 to meet national demand, that means we’re operating at just 26.6% capacity,” Arianti said.
Microbiological diagnosis plays a vital role in helping pulmonologists determine the most effective treatment plans. Without adequate lab personnel, delayed diagnoses and treatments are more likely, contributing to the continued spread of TB, especially drug-resistant strains.
(Raidi/Agung)